Suzuki discovered the enzyme NGLY1 and its gene in the 1990s and explored its biological function, but did not anticipate that is would be related to any human disease. First discovered in the United States in 2012, NGLY1 deficiency is a life-threatening disorder. Patients exhibit severe symptoms such as developmental and intellectual delays, decreased limb strength, the inability to produce tears, involuntary movements, and seizures. Life expectancy is not known because of the small number of patients, but some die in their teens or earlier through a variety of immediate causes. Since then, Suzuki and his lab have been researching ways to treat this rare disease.
What makes the disease particularly difficult is that it has only been confirmed in 100 or so patients worldwide, though researchers suspect that many cases may not be properly diagnosed — meaning it might be more common than it seems.
“We are dealing with a rare disease that is confirmed to affect only around one hundred patients globally. However, I don’t think that means that fundamental research leading to treatment is any less important,” emphasizes Suzuki.
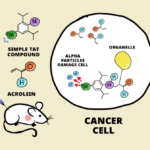
According to Suzuki, although there is still a lot that is not understood about NGLY1 deficiency, we do know that the affected gene codes for an enzyme that helps remove a specific type of glycan (sugar molecule) from the surface of proteins. Recently, Suzuki’s team came up with a surprising finding that might be able to help the patients. His group has been collaborating with a pharmaceutical company to develop treatments for NGLY1 deficiency, and they established NGLY1-deficient rat and mouse models for their studies.
Pharmaceutical companies tend to be reluctant to conduct research on rare diseases, but a program called the Takeda-CiRA Joint Programme for iPS Cell Applications (T-CiRA) has made the collaboration possible. The T-CiRA project is a collaborative initiative between academia and industry focused on advancing regenerative medicine using iPS cells, which aims to develop innovative treatments for diseases – even rare diseases – by translating iPS cell research into clinical applications. The project invited Suzuki to join because he was already conducting research on NGLY1 in Japan, making him the ideal candidate for the collaboration. “I honestly wasn’t sure if I would be able to carry out the research successfully, having never used iPS cells before. But the director, Dr Yamanaka, encouraged me, saying that I would do well because of my ‘NGLY1 love’,” recalls Suzuki.
In a recent study published in Communications Biology, Suzuki’s team analyzed the mouse model of NGLY1 deficiency, finding that it exhibited seizure-like symptoms 30-40 times a day. In an effort to identify the cause, they measured gene expression in the model mouse brains and spinal cords and discovered a gene whose expression was reduced in the hypothalamus. The identity of this gene was quite a surprise.
What gene was it? It turns out it was the gene that codes for oxytocin, a neuropeptide known as the “love hormone.” “This gene had never been reported to be associated with NGLY1, so this result was a surprise,” says Suzuki. Oxytocin has also been reported to affect social behavior, so perhaps, they thought, it could be related to the social impairments seen in patients.
Naturally, Suzuki’s team wondered whether supplementing oxytocin to the brain could improve the seizure-like symptoms in the model mice. The team sprayed oxytocin into the noses of the mice and confirmed that this led to higher levels of oxytocin in the blood and brain. As they had hoped, their intervention temporarily suppressed the seizure-like symptoms for at least 4 hours.
The next question, of course, is whether this can work in humans, which would demonstrate that their mouse model is clinically relevant. “Oxytocin has already been approved for use as a drug for inducing labor, so we figured that if its application could be expanded to suppressing seizures in NGLY1 deficiency, it could quickly become a new treatment option,” explains Suzuki.
The road ahead is not without challenges, however. First, the group has to find out whether oxytocin levels are reduced in human patients who exhibit seizures. Unfortunately, obtaining serum samples is difficult due to the rarity of the disease and the small number of surviving patients. Additionally, oxytocin levels in humans are lower than in mice, making it difficult to measure.
In fact, Suzuki says that that getting this information is impossible unless clinical doctors are proactive about administering oxytocin. However, based on his discussions with several clinicians around the world, only a few were optimistic about making an Investigational New Drug application to the FDA for oxytocin treatment in clinical trials. Since clear effects were observed in the crossover trial, the researchers are quite confident about the drug’s efficacy in mice. “It is our earnest wish to confirm whether oxytocin levels are decreased in patients and, if possible, to administer it to them, but there is no prospect of this happening in the near future.”
“Drug-treatment research for rare diseases may not be attractive from the perspective of efficiency and profitability, but we now know that we have a potential treatment, and we haven’t given up the hope of finding out whether it will be effective in humans.”
Further reading
Makita Y, Asahina M, Fujinawa R, Yukitake H, Suzuki T (2024) Intranasal oxytocin suppresses seizure-like behaviors in a mouse model of NGLY1 deficiency. Commun Biol. doi:10.1038/s42003-024-06131-7
Makita Y, Asahina M, Fujinawa R, Yukitake H, Suzuki T (2024) Intranasal oxytocin suppresses seizure-like behaviors in a mouse model of NGLY1 deficiency. Commun Biol. doi:10.1038/s42003-024-06131-7