A molecular signaling pathway linked to psychiatric symptoms in Huntington’s disease has been identified RIKEN researchers. This discovery could offer fresh insights into not just Huntington’s disease but also mental illness more generally.
A hereditary neurological condition that gets progressively worse, Huntington’s disease is mainly characterized by involuntary, dance-like movements. It is caused by mutations in the Huntingtin (HTT) gene, which result in the production of misfolded Huntingtin protein molecules. These molecules aggregate to form insoluble clumps, leading to nerve cell death in the striatum—a region of the brain involved in voluntary movements.
Huntington’s disease has traditionally been considered a movement disorder, but its classic symptoms are now known to be accompanied by psychiatric ones, particularly depression. Very little is known about the underlying molecular mechanisms for these symptoms, however.
Motomasa Tanaka at RIKEN Brain Science Institute and his colleagues examined genetically engineered mice carrying a mutated human HTT gene. These mice exhibited the pathological hallmarks of Huntington’s disease, including HTT aggregation.
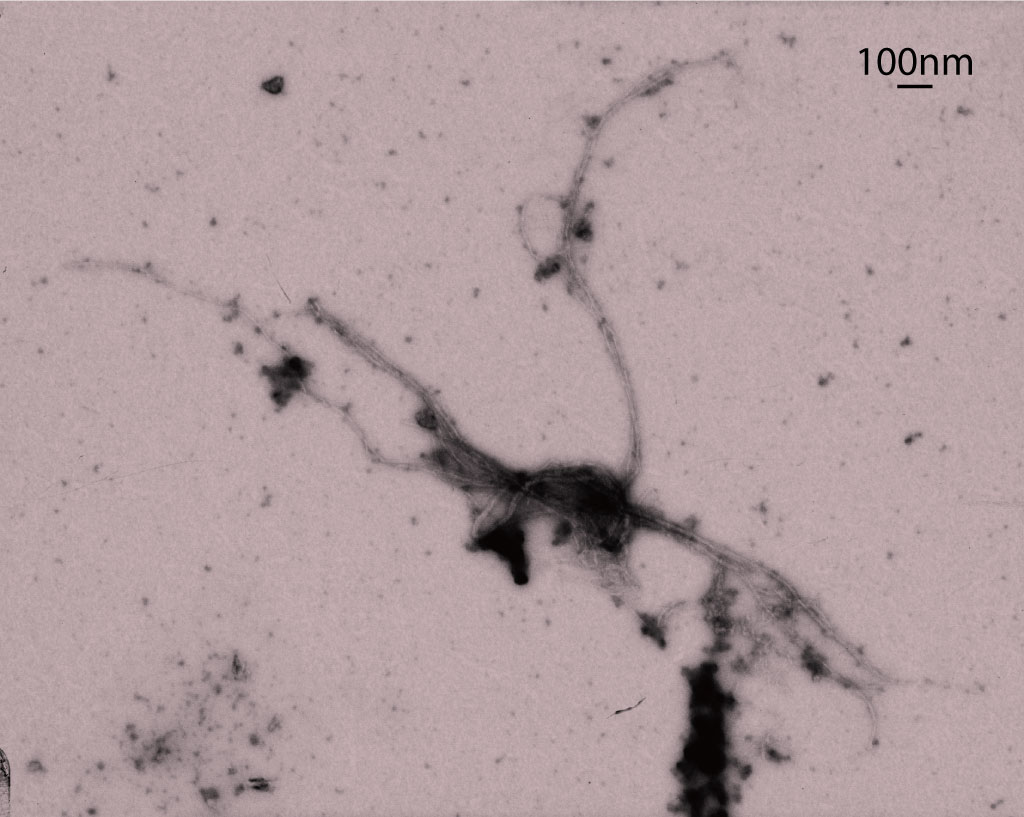
Transmission electron microscopy image of a DISC1 aggregate.
Republished with permission of American Society for Clinical Investigation, from Ref. 1; permission conveyed through Copyright Clearance Center, Inc.
The researchers performed a series of biochemical assays and found that misfolded HTT protein binds to another cellular protein called DISC1, causing them to aggregate (Fig. 1). This boosts the activity of PDE4—an enzyme that breaks down a small signaling molecule called cAMP. DISC1 normally binds to PDE4 to restrict its activity, but in Huntington’s disease it binds to HTT instead. Consequently, PDE4 becomes overactive, leading to reduced cAMP levels.
The team then examined brain tissue samples obtained from Huntington’s disease patients after death and found that they too contained insoluble clumps made of mutant HTT protein bound to DISC1. In contrast, tissue samples from three individuals who died of other causes did not contain these aggregates.
Behavioral testing further revealed that the mutant mice showed no preference for a sugar solution over water, indicating that they have anhedonia, or an inability to experience pleasure and reward, one symptom of depression. However, their preference for the sweet drink could be restored by injecting them with a shortened form of DISC1 that does not bind to mutant HTT restored. This suggests that the alterations in this signaling pathway are associated with anhedonia.
“Reduced levels of soluble, functional DISC1 due to co-aggregation with HHT is responsible for anhedonia in Huntington’s disease,” says Tanaka, “so DISC1 supplements could reduce this symptom.”
“This study leaves a critical question unanswered,” he adds. “Can our co-aggregation hypothesis explain diverse psychiatric symptoms, including social deficits, in other neurodegenerative diseases? We are keen to investigate this.” ?
[vifblike]
This article originally appeared here as a RIKEN Research Highlight.
A molecular signaling pathway linked to psychiatric symptoms in Huntington’s disease has been identified RIKEN researchers. This discovery could offer fresh insights into not just Huntington’s disease but also mental illness more generally.
A hereditary neurological condition that gets progressively worse, Huntington’s disease is mainly characterized by involuntary, dance-like movements. It is caused by mutations in the Huntingtin (HTT) gene, which result in the production of misfolded Huntingtin protein molecules. These molecules aggregate to form insoluble clumps, leading to nerve cell death in the striatum—a region of the brain involved in voluntary movements.
Huntington’s disease has traditionally been considered a movement disorder, but its classic symptoms are now known to be accompanied by psychiatric ones, particularly depression. Very little is known about the underlying molecular mechanisms for these symptoms, however.
Motomasa Tanaka at RIKEN Brain Science Institute and his colleagues examined genetically engineered mice carrying a mutated human HTT gene. These mice exhibited the pathological hallmarks of Huntington’s disease, including HTT aggregation.
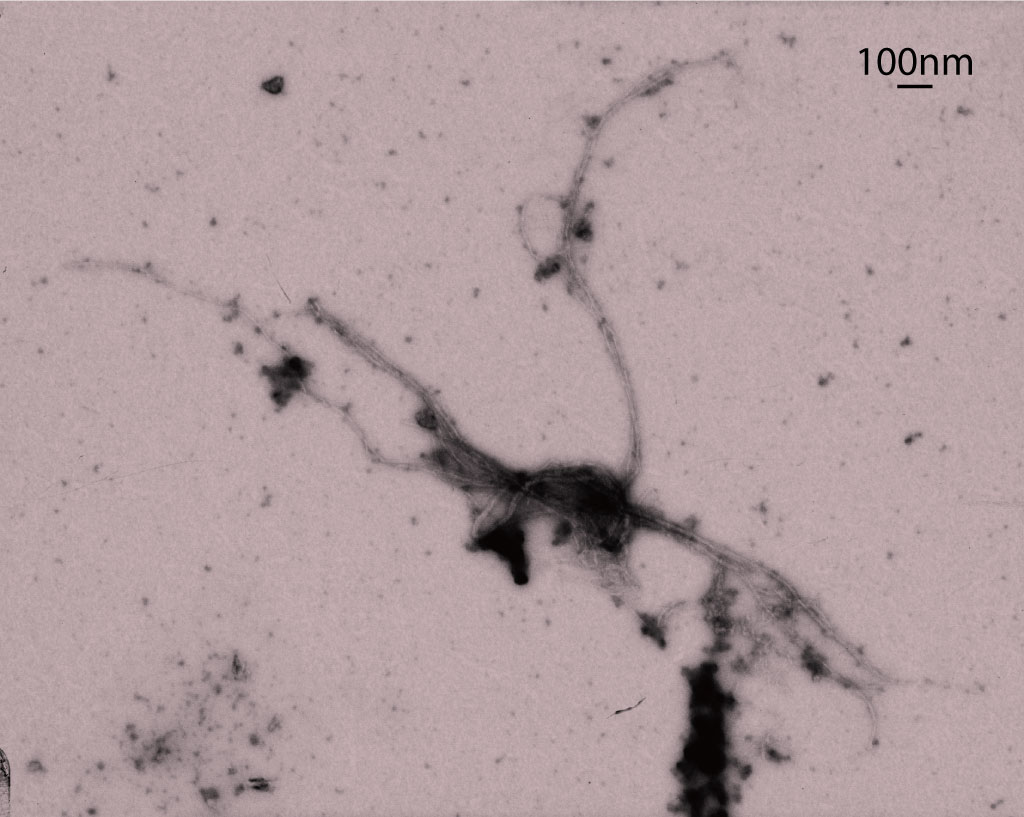
Transmission electron microscopy image of a DISC1 aggregate.
Republished with permission of American Society for Clinical Investigation, from Ref. 1; permission conveyed through Copyright Clearance Center, Inc.
The researchers performed a series of biochemical assays and found that misfolded HTT protein binds to another cellular protein called DISC1, causing them to aggregate (Fig. 1). This boosts the activity of PDE4—an enzyme that breaks down a small signaling molecule called cAMP. DISC1 normally binds to PDE4 to restrict its activity, but in Huntington’s disease it binds to HTT instead. Consequently, PDE4 becomes overactive, leading to reduced cAMP levels.
The team then examined brain tissue samples obtained from Huntington’s disease patients after death and found that they too contained insoluble clumps made of mutant HTT protein bound to DISC1. In contrast, tissue samples from three individuals who died of other causes did not contain these aggregates.
Behavioral testing further revealed that the mutant mice showed no preference for a sugar solution over water, indicating that they have anhedonia, or an inability to experience pleasure and reward, one symptom of depression. However, their preference for the sweet drink could be restored by injecting them with a shortened form of DISC1 that does not bind to mutant HTT restored. This suggests that the alterations in this signaling pathway are associated with anhedonia.
“Reduced levels of soluble, functional DISC1 due to co-aggregation with HHT is responsible for anhedonia in Huntington’s disease,” says Tanaka, “so DISC1 supplements could reduce this symptom.”
“This study leaves a critical question unanswered,” he adds. “Can our co-aggregation hypothesis explain diverse psychiatric symptoms, including social deficits, in other neurodegenerative diseases? We are keen to investigate this.” ?
[vifblike]
This article originally appeared here as a RIKEN Research Highlight.
Tanaka M et al. (2017) Aggregation of scaffolding protein DISC1 dysregulates phosphodiesterase 4 in Huntington’s disease. J Clin Invest. 127:1438–1450. doi: 10.1172/JCI85594
[yuzo_related]